|
 |
- Search
| J Korean Med Assoc > Volume 54(2); 2011 > Article |
Abstract
Despite the recent increase in the use of complementary and alternative medicine (CAM) among the general population and patients, little is known about Korean physicians' attitudes about and interest in CAM. We conducted a web-based survey of knowledge, attitude, and experience in CAM among primary care physicians (PCPs) and academic physicians (APs) in Korea. A total of 826 physicians (341 PCPs and 485 APs) responded. Respondents in both groups felt that they were not sufficiently knowledgeable about CAM. PCPs, however, had a significantly higher composite index score in CAM knowledge than that of APs. Although APs were more skeptical about the scientific evidence of CAM than PCPs, both groups had a positive attitude toward CAM. The level of experience in utilizing CAM in their practice was 23.2% among PCPs, which was much higher than that among APs (2.7%). Experience rates of referring patients to CAM were 11.7% in PCPs and 4.5% in APs (P<0.001). Despite the discrepant rates in CAM education between the two groups (58.7% in PCPs and 26.0% in APs, P<0.001), the majority of doctors in both groups (85.0% in PCPs and 70.0% in APs) expressed an intention to participate in authorized CAM coursework. In conclusion, despite the lack of scientific evidence, both PCPs and APs have an interest in incorporating CAM into their conventional medical practices. To meet physicians' increasing needs for CAM the Korean medical societies should promote education and research about CAM in the conventional medical system.
With a worldwide increase in the use of complementary and alternative medicine (CAM) among the general population [1-4] as well as among medical patients [5-7], the perspective of the medical community has been changing [8-9]. In Korea, the annual utilization rate of CAM among adults has progressively increased from 29% in 1999 [10] to 74.8% in 2006 [11].
Until now, however, Korean physicians' opinions about and behaviors regarding CAM have not been sys-tematically examined, except for one study published in 2002 [12] which surveyed conventional-medicine-trained doctors (MDs) and Oriental-medicine-trained doctors (OMDs). That study showed that OMDs had more knowledge of and experience with favorable attitudes regarding CAM than MDs did. That may be due to the common background of Oriental medicine and CAM in terms of philosophy and practice [13].
On that basis, it is reasonable to focus on the MDs' per spective on accepting CAM in the Korean medical system. According to a previous survey of general practitioners and hospital doctors [14], the former had more experience with CAM than the latter. Although no study has compared primary care physicians (PCPs) and academic physicians (APs), it is possible to hypothesize that PCPs are more open to CAM than APs, physicians that place an emphasis on scientific evidence in their practice. This possible discrepancy may result in differences in the behaviors of these two physician groups. For the first time in Korea, this study compares the knowledge, attitude, and experience in CAM between PCPs and APs.
The study subjects were divided into two groups: PCPs located throughout Korea and APs at the Seoul National University Hospital and its three affiliated hospitals. E-mails linked to an anonymous, web-based survey site were sent to each group for 1 month from December 2008 to February 2009. The survey was delivered to PCPs by a 'news ticker' on the screen of an electronic medical record (EMR) system (Ysarang; UBCare Co., Seoul, Korea), a widely used EMR system covering about 20% of primary care clinics in Korea at the time of this survey (calculated using the number of subscribers and data from medical care institutions in the 2008 National Health Insurance Statistics [15]). In Korea, PCPs include not only general practitioners but also almost all specialist categories.
The APs consisted of interns, residents, fellows, and faculty members. For those surveys, the survey invitations were e-mailed to each subject three times, at one week intervals. Each invitation included a coupon for a free coffee or tea at a list of designated shops.
The questionnaire comprised four sections: 1) knowledge about CAM, 2) attitude toward CAM, 3) experience in education about CAM and experience with clinical practice in CAM, and 4) socio-demographic variables including age, sex, years of practice, specialty, and region. A pilot test was done by 20 physicians to verify the validity and reliability of the method, but that test was limited in scope. Approximately 10 minutes was required to complete the questionnaire, which was designed such that all questions required an answer.
To evaluate physicians' knowledge about CAM, we listed 15 CAM modalities (Figure 1). Answers were framed within a five-point Likert scale from 1 (not known at all) to 5 (know very well). The attitude portion of the questionnaire consisted of 24 statements that were modified from previous studies [16-19]. These statements were divided into 6 categories according to similarities in concept. The questions allowed answers for each statement that were classified as strongly agree, agree, neutral, disagree, strongly disagree, and cannot judge.
The questionnaire items related to CAM experience included questions regarding physicians' experiences with being asked about CAM from patients as well as regarding experiences with recommending CAM use, including preparing patient referrals to CAM practitioners. In addition, we asked about physicians' experiences with CAM training and about their intention to obtain CAM-related education.
We used SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA) for statistical analysis. Independent t-tests for continuous data and Pearson χ2-tests for nominal data were used when comparing knowledge, attitude, and behavior between PCPs and APs. A probability P-value of less than 0.05 was considered significant.
Responses were obtained from 341 PCPs (estimated to be a 3% response rate) and 485 APs (a 25.1% response rate). The mean (±SD) age of the respondents was 44.3±7.3 years for the PCPs and 32.6±6.6 years for the APs; a significant difference (P<0.001). The mean practice duration was 17.4±7.5 years for PCPs and 7.19±6.56 for APs (P<0.001). The male to female ratio of the PCP respondents was significantly different from that of the AP respondents (6.1:1 vs. 1.4:1, respectively) (P<0.001). Among the various positions occupied by the APs, the response rate among fellows (123/227, 54.2%) was the highest, followed by interns (62/200, 31%), residents (181/810, 22.3%), and faculty members (113/693, 16.3%), with the response rates showing a significantly different distribution from that expected (P<0.001) (Table 1).
A summary of the physicians' responses to questions regarding knowledge about CAM is shown in Figure 1. In both groups, the overall physicians' level of knowledge for CAM was low. Average scores for each item were under 3.0 (median score in the 5-point Likert scale) except for two items: dietary supplements or functional foods and intramuscular stimulation (IMS) with scores of 3.17 and 3.21, respectively, in the PCP group. We calculated the composite index of CAM knowledge by summing all scores across the 15 CAM modalities. The composite indices were 35.94 (95% confidence interval [CI], 34.95-36.93) for PCPs and 34.51 (95% CI, 33.76-35.26) for APs. Both were lower than the neutral value of 45 (i.e., median score 3×15 items) (P<0.001 in both groups). Overall, PCPs were significantly more knowledgeable than APs in the composite index of CAM knowledge (P=0.02). With regard to the knowledge of acupuncture/moxibustion, dietary supplements or functional foods, manipulative therapies, and IMS, PCPs had significantly higher average scores than APs (all P<0.01) (Figure 1). The CAM modalities for which APs showed superior knowledge compared to that of PCPs were biofeedback or neurofeedback, meditation or relaxation therapy, and art or music therapy. The energy healing therapy category received the lowest knowledge score in both groups. CAM knowledge scores were not significantly related to other demographic factors such as age, sex, and practice period for both groups.
Statements exhibiting anti-CAM beliefs were reversely scored in order to appropriately reflect positive and negative attitudes within the statements. The five-point scale from 1 (strongly disagreeing with a positive statement, or strongly agreeing with a negative statement) to 5 (strongly agreeing with a positive statement, or strongly disagreeing with a negative statement) was used to score each answer. The response 'cannot judge' was treated as missing data and was not assigned a value. A summary of the respondents' attitude responses is shown in Table 2.
The composite attitude indices were 75.81 (95% CI, 74.29-77.33) for PCPs and 72.85 (95% CI, 71.88-73.82) for the APs. The composite index of PCPs was significantly higher than both the neutral value of 72 (median score 3×24 items) (P<0.001) and that of APs. On the other hand, overall attitude of the APs was slightly positive, but the difference was not statistically significant (P=0.09).
Most physicians strongly supported the philosophical statements such that regarding the influence of mental health and health beliefs (PCPs, 4.14; APs, 4.12; statement 3)(Table 2), the body's self healing mechanism (PCPs, 3.90; APs, 3.64; statement 2), and vital energy or force (PCPs, 3.28; APs, 2.97; statement 1). The results, however, revealed skepticism regarding the scientific reliability of CAM. Both groups thought that CAM is unreliable (PCPs, 2.48; APs, 2.28; statement 6) and fairly unscientific (PCPs, 2.86; APs, 2.68; statement 5) so its evidence should be proven by rigorous research methods (PCPs, 2.72; APs, 2.68; statement 4) The skeptical opinion tendency was more prominent in APs than PCPs.
Both groups showed a neutral opinion to statement 7 regarding CAM's placebo effects (PCPs, 3.10; APs, 2.97), and thought that it is difficult to estimate CAM's own effect (PCPs, 2.51; APs, 2.27; statement 10) and expressed concern over statement 13 regarding possible side effects of CAM (PCPs, 2.55; APs, 2.36). Although APs disagreed more than the PCPs with statement 20 that CAM is merely a fashionable fad which will soon disappear (PCPs, 3.45 vs. APs, 3.57; P=0.04), they revealed more hesitation regarding concurrent treatment with orthodox medicine and CAM (PCPs, 3.29 vs. APs, 3.08; P=0.001). On the topic of the necessity of CAM education, both groups expressed significantly higher demands in three related questions (statements 21-23) (Table 2).
Among the specialties, family medicine physicians had a significantly high composite CAM attitude index (PCPs, 79.5; APs, 82.89), both of which were significantly greater than the neutral value (each P<0.001). Among PCPs, females exhibited significantly more positive attitude than males (82.1 vs. 74.8, respectively; P=0.001). On the other hand, APs showed no gender difference (females, 73.7 vs. males, 72.2; P=0.14). The composite CAM attitude indices were not significantly correlated to other demographic factors such as age, position, and practice period.
Figure 2 summarizes the results of CAM questions regarding patients' requests, doctors' recommendations, doctors' experiences, and doctors' wishes to learn. A majority of the physicians (PCPs, 82%; APs. 82.5%) had previously been asked about the use of CAM by their patients. The most common CAM modality requested by patients was herbal medicine or animal extracts (PCPs, 28.2%; APs, 40.1%) followed by acupuncture or moxibustion (PCPs, 26.8%; APs, 20.3%) and dietary supplements or functional foods (PCPs, 22.5%; APs, 29.1%). Regarding the patients' use of CAM, 27.4% of PCPs and 10.8% of APs reported that they responded positively. In contrast, Figure 3 shows that more physicians in both group answered that they would respond positively to a request regarding an acquaintance's use of CAM (PCPs, 51.9%; APs, 37.5%).
Thirty nine percent of PCPs and 13.8% of APs had previously recommended CAM to their patients before the patients requested such treatment; the difference between the two groups was significant (P<0.001). Provision of dietary supplements or functional foods was the most recommended modality in both groups (PCPs, 29.8%; APs, 17.8%). The next two most requested modalities were IMS (21.1%) and acupuncture/moxibustion (8.7%) among PCPs and meditation and relaxation therapy (16.3%) and IMS (13.2%) among APs (Figure 2).
The referral rates to CAM practice were very low in both groups, but PCPs had relatively more experience in practicing CAM than APs did. A significantly higher percentage of PCPs (23.2%) than APs (2.7%) had experience in providing CAM (P<0.001). Also a significantly higher percentage of PCPs (11.7%) than APs (4.5%) had experience in referring patients to CAM treatment (P<0.001). Among both PCPs and APs there were no significant differences found in age and practice period when comparing physicians with and without experiences in CAM practice or referral. On the other hand, female PCPs referred significantly more patients to CAM than male PCPs did (female, 20.8% vs. male, 10.2%; P=0.03). This gender-related difference was not found among APs.
PCPs received significantly more education in CAM than APs (58.7% vs. 26.0%, respectively; P<0.001). The most common CAM modalities in which physicians received training are shown in Figure 2. Regarding the source of the learning, undergraduate courses were responsible for only 1% of the training for PCPs and 6.6% for APs, who were all interns or residents when receiving their training. The majority of physicians in both groups learned CAM through continuing medical education courses offered by academic societies. Neither PCPs nor APs showed significant differences in age and practice period when comparing physicians who had CAM education to those who did not.
The majority of the respondents (PCPs, 85.0%; APs, 70.0%) expressed intention to participate in authorized CAM education coursework, if such courses were provided by academic medical society. The CAM modalities that physicians preferred to learn were IMS, dietary supplements or functional foods, herbal medicine or animal extract, and acupuncture/moxibustion (Figure 2).
Age and practice period were neither related to experience in education nor to the intention to obtain education about CAM in both groups. Significant gender differences were found in the training experience in PCPs (male, 56.3% vs. female, 72.9%; P=0.03), and in the intention to obtain education in APs (male, 65.6% vs. female, 75.4%; P=0.02).
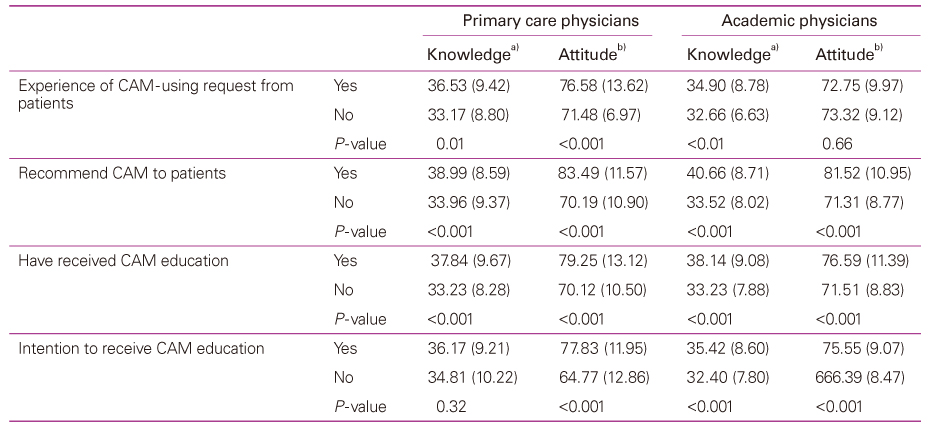
Correlation analyses indicated that physicians who felt more knowledgeable were likely to have more positive attitudes toward CAM in both groups (correlation coefficient r=0.23 in PCPs and 0.32 in APs; P<0.001 in both groups). Both CAM knowledge and CAM attitude were significantly related to the physicians' behaviors regarding CAM (Table 3) in both groups. PCPs who had received inquiries about CAM from their patients had significantly higher scores in the composite index of CAM knowledge and attitude than those who had not been asked. However, APs only showed such a tendency in the knowledge index, in spite of the similarity between the two groups in experience with their patients' CAM use requests. Moreover, not only did the physicians who had more experience in recommendation and education about CAM, but also those who had more intention to receive CAM education had significantly higher scores in knowledge and attitude indices.
PCPs are more practice-oriented and are confronted with a greater variety of patients' demands than APs. On the other hand, APs emphasize the need for scientific evidence, which makes them be more reluctant to accept new concepts, such as CAM. However, considering that APs have a substantial impact on research, medical practice, and medical education related to CAM [20], it is reasonable to survey and compare APs and PCPs. For this reason we compared the knowledge, attitude, and experience in CAM between PCPs and APs in Korea.
In general, although their subjective levels of CAM knowledge were low, this study's results show that both PCPs and APs had a positive attitude toward CAM. Not surprisingly, physicians who had higher knowledge and more positive attitude toward CAM were much more likely to have experience in CAM, such as recommending CAM treatment or obtaining education in CAM. These results are similar with those in previous studies [12,20,21]. Taken together, these results emphasize the importance of CAM education in physicians' use of CAM in the future.
As we hypothesized, PCPs possessed more positive attitude, more knowledge, and greater levels of experience regarding CAM than APs. That result is also similar to previous surveys. One United Kingdom survey indicated that general medical practitioners were superior to hospital-based doctors in knowledge, attitude, and experience related to CAM [14]. Another national survey in Germany reported that PCPs were significantly more inclined to use CAM than specialists were [22].
Increased open communications between doctors and patients about CAM may enhance a doctors' knowledge of or possibly affect their attitude toward CAM [23]. According to another United Kingdom survey, the main reason for referring patients to CAM by primary care workers was due to patients' requests [24]. Similarly, this study showed that the physicians who had previous experience with CAM requests from their patients were more knowledgeable and positive about CAM. On the other hand, unlike PCPs, APs' attitude was not affected by such experience (Table 3). This suggests that APs, presumably because of their more negative views of CAM's scientific reliability than those of PCPs, are more reluctant to recommend CAM treatment despite their patients' demand. From these results and on the basis of previous surveys [20,21,23,24], we hypothesize that patients'inquiries about CAM use will enhance physicians' knowledge, either through self-directed learning or other forms of education, and will encourage them to use or recommend CAM in their practice. However, it is difficult to distinguish cause-and-effect relationships between variables in this cross-sectional type study; thus future longitudinal studies are needed to test our hypothesis.
Interestingly, we found some discrepancies between patients'needs and physicians' responses, which were more prominent among APs. First, we detected a discrepancy between what patients most commonly asked about and what physicians knew well. The former were herbal medicine or animal extracts, acupuncture/moxibustion, and dietary supplements or functional foods while the latter were dietary supplements or functional foods and IMS for both PCP and AP groups. Furthermore, those two forms of CAM (i.e., dietary supplements or functional foods and IMS) were what both groups of physicians most commonly recommended to patients and had training in. Figuratively speaking, both herbal medicine and acupuncture have become acculturated to dietary supplements (vitamins, minerals, etc.) and IMS, respectively. Actually, dietary supplements are becoming generally considered to be very close to conventional medicine rather than to CAM. Furthermore, there is controversy over whether IMS is to be considered as CAM or not, because many physicians who specialize in IMS insist that it is a kind of conventional medical treatment that is based on modern anatomy and physiology. In Korea, such a discrepancy may be related to the dual healthcare system, in which conventional medicine-trained doctors are legally prohibited from practicing Oriental medicine, such as herbal medicine or acupuncture. In contrast, a survey at the Johns Hopkins Medical Institute reported that their physicians had the highest CAM knowledge level (90%) in acupuncture [25]. In other Western countries, acupuncture is one of the major CAM modalities that physicians prefer to use [22,24].
Although the majority of physicians (more than 82% in both groups) had previously been asked about CAM use by their patients, the referral rates (PCPs, 23.2%; APs, 2.7%) and the practice rates (PCPs, 11.7%; APs, 4.5%) were much lower than those reported in Western countries [16,21,26]. These discrepancies between patients'needs and doctors' behaviors may be related to an underdeveloped referral or communication system between doctors and CAM practitioners, including OMDs. Another reason attributed to this lower rate of CAM use may be due to the fact that Oriental medicine is competitively positioned opposite conventional medicine in Korea [12].
Finally, the result that physicians respond more positively to their acquaintances'CAM use than to their patients' use reflects a tendency within the patient-doctor discrepancy and this tendency was more prominent among APs. This may be related to the results in this study which indicated that APs place more emphasis than PCPs on the scientific reliability of CAM. Our results appear to support those in a United States survey where the rate of private CAM use by faculty members working in a health science center (52%) was similar to that within the general population (52%) [27].
Most published surveys have reported that a high percentage of physicians (62% to 84%) want to receive education in CAM [28-30]. In our study, 85% of the PCPs and 70% of the APs expressed such an intention. The results that physicians who received undergraduate education of CAM were all interns or residents, is an indication that CAM education during medical school has been done only for a recent few years. According to a recent survey about Korean faculties in family medicine, most of the faculty members (77.6%) recognized the need for providing CAM education to their family medicine residents [31]. The authors, however, pointed out that the lack of a training infrastructure would be an obstacle to increasing CAM education. Such education can improve the knowledge burden which physicians undertake when they are asked about CAM by patients. This suggests that such an unmet need in physicians should be resolved by modification of the education system.
There are some limitations in this study. First, randomized sampling was not done within the two physician groups. For example, age distribution was significantly different between the two groups. Moreover, it was not possible to determine an exact response rate for PCPs due to a defect in the delivery of the survey, and the AP group was sampled from only one university hospital and its three affiliated hosptals. These samples, therefore, might not represent the entire Korean PCP and AP populations. Second, bias may have entered the survey if respondents with more positive or more negative attitude toward CAM participated to a greater extent than other respondents. The presence or severity of such bias is unknown, but it is possible that the respondents in this study were not representative of the target population. Third, this study was cross-sectional rather than longitudinal. Therefore, it cannot produce causal inferences from our analyses. As a result, caution is required when formulating conclusions from this study. Despite these limitations, our results are meaningful because this is the first systematic survey about the knowledge, attitudes, and experience about CAM among PCPs and APs in Korea.
There are discrepancies between patients' demands and physicians' responses regarding CAM use, and between the reality of current CAM education levels and physicians' need for such education. The study indicates that many Korean physicians feel that they should be better informed about CAM. To meet these increasing needs for CAM in physicians, the Korean medical societies should promote education and research about CAM in the conventional medical system. More extensive, quantitative and qualitative studies are recommended in order to identify further the important factors affecting CAM behavior of physicians in the near future.
Acknowledgement
We would like to thank the Seoul National Univer-sity Hospital Cyber Academy and UBCare Co. for deli-vering the survey questionnaire to doctors. No com-peting financial interests exist.
References
1. Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data 2004;343):1-19.
2. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report 2008;12):1-23.
3. Xue CC, Zhang AL, Lin V, Da Costa C, Story DF. Complementary and alternative medicine use in Australia: a national population-based survey. J Altern Complement Med 2007;13:643-650.
4. Härtel U, Volger E. Use and acceptance of classical natural and alternative medicine in Germany: findings of a representative population-based survey. Forsch Komplementarmed Klass Naturheilkd 2004;11:327-334.
5. Saydah SH, Eberhardt MS. Use of complementary and alternative medicine among adults with chronic diseases: United States 2002. J Altern Complement Med 2006;12:805-812.
6. Artus M, Croft P, Lewis M. The use of CAM and conventional treatments among primary care consulters with chronic musculoskeletal pain. BMC Fam Pract 2007;8:26.
7. Corner J, Yardley J, Maher EJ, Roffe L, Young T, Maslin-Prothero S, Gwilliam C, Haviland J, Lewith G. Patterns of complementary and alternative medicine use among patients undergoing cancer treatment. Eur J Cancer Care (Engl) 2009;18:271-279.
8. Astin JA, Marie A, Pelletier KR, Hansen E, Haskell WL. A review of the incorporation of complementary and alternative medicine by mainstream physicians. Arch Intern Med 1998;158:2303-2310.
9. Hsiao AF, Ryan GW, Hays RD, Coulter ID, Andersen RM, Wenger NS. Variations in provider conceptions of integrative medicine. Soc Sci Med 2006;62:2973-2987.
10. Lee SI, Khang YH, Lee MS, Koo HJ, Kang W, Hong CD. Complementary and alternative medicine use in Korea: prevalence, pattern of use, and out-of-pocket expenditures. Korean J Prev Med 1999;32:546-555.
11. Ock SM, Choi JY, Cha YS, Lee J, Chun MS, Huh CH, Lee SY, Lee SJ. The use of complementary and alternative medicine in a general population in South Korea: results from a national survey in 2006. J Korean Med Sci 2009;24:1-6.
12. Lee SI, Khang YH, Lee MS, Kang W. Knowledge of, attitudes toward, and experience of complementary and alternative medicine in western medicine-and oriental medicine-trained physicians in Korea. Am J Public Health 2002;92:1994-2000.
13. Hong CD. Complementary and alternative medicine in Korea: current status and future prospects. J Altern Complement Med 2001;7 Suppl 1:S33-S40.
14. Perkin MR, Pearcy RM, Fraser JS. A comparison of the attitudes shown by general practitioners, hospital doctors and medical students towards alternative medicine. J R Soc Med 1994;87:523-525.
15. National Health Insurance Corporation, Health Insurance Review & Assessment Service. 2008 National Health Insurance statistics 2009;Seoul: National Health Insurance Corporation, Health Insurance Review & Assessment Service.
16. Lewith GT, Hyland M, Gray SF. Attitudes to and use of complementary medicine among physicians in the United Kingdom. Complement Ther Med 2001;9:167-172.
17. Hyland ME, Lewith GT, Westoby C. Developing a measure of attitudes: the holistic complementary and alternative medicine questionnaire. Complement Ther Med 2003;11:33-38.
18. Schneider CD, Meek PM, Bell IR. Development and validation of IMAQ: Integrative Medicine Attitude Questionnaire. BMC Med Educ 2003;3:5.
19. Furnham A, McGill C. Medical students attitudes' about complementary and alternative medicine. J Altern Complement Med 2003;9:275-284.
20. Rosenbaum ME, Nisly NL, Ferguson KJ, Kligman EW. Academic physicians and complementary and alternative medicine: an institutional survey. Am J Med Qual 2002;17:3-9.
21. Berman BM, Singh BB, Hartnoll SM, Singh BK, Reilly D. Primary care physicians and complementary-alternative medicine: training, attitudes, and practice patterns. J Am Board Fam Pract 1998;11:272-281.
22. Stange R, Amhof R, Moebus S. Complementary and alternative medicine: attitudes and patterns of use by German physicians in a national survey. J Altern Complement Med 2008;14:1255-1261.
23. Maha N, Shaw A. Academic doctors' views of complementary and alternative medicine (CAM) and its role within the NHS: an exploratory qualitative study. BMC Complement Altern Med 2007;7:17.
24. van Haselen RA, Reiber U, Nickel I, Jakob A, Fisher PA. Providing complementary and alternative medicine in primary care: the primary care workers' perspective. Complement Ther Med 2004;12:6-16.
25. Song MY, John M, Dobs AS. Clinicians' attitudes and usage of complementary and alternative integrative medicine: a survey at the Johns Hopkins Medical Institute. J Altern Complement Med 2007;13:305-306.
26. Joos S, Musselmann B, Szecsenyi J. Integration of complementary and alternative medicine into family practices in Germany: results of a national survey. Evid Based Complement Alternat Med 2011;2011:495813. DOI: 10.1093/ecam/nep019.
27. Burg MA, Kosch SG, Neims AH, Stoller EP. Personal use of alternative medicine therapies by health science center faculty. JAMA 1998;280:1563.
28. Milden SP, Stokols D. Physicians' attitudes and practices regarding complementary and alternative medicine. Behav Med 2004;30:73-82.
29. Levine SM, Weber-Levine ML, Mayberry RM. Complementary and alternative medical practices: training, experience, and attitudes of a primary care medical school faculty. J Am Board Fam Pract 2003;16:318-326.
30. Corbin Winslow L, Shapiro H. Physicians want education about complementary and alternative medicine to enhance communication with their patients. Arch Intern Med 2002;162:1176-1181.
31. Ock SM, Kim CM, Choi WS, Ju SY, Shin HC, Song CH. Perception and experience of CAM education for family practice residents by family practice training faculty in South Korea. J Korean Acad Fam Med 2008;29:932-938.
Figure 1
Comparison of knowledge about complementary and alternative medicine (CAM) between primary care physicians and academic physicians. 5-Point scale of CAM knowledge (from 1 [I don't know at all] to 5 [I know very well]). *P<0.001, **P<0.01, and ***P<0.05 for comparison between primary care physicians and academic physicians. a)Chiropractic, osteopathy, Tui Na, massage, etc. b)Electromagnetic field, wave, Qi therapy, etc. c)Yoga, Tai chi, Qigong, etc. d)Prayer, beliefs, spirituality, etc. e)Organic food, wood bathing, etc. f)Colon cleansing, chelation, etc.
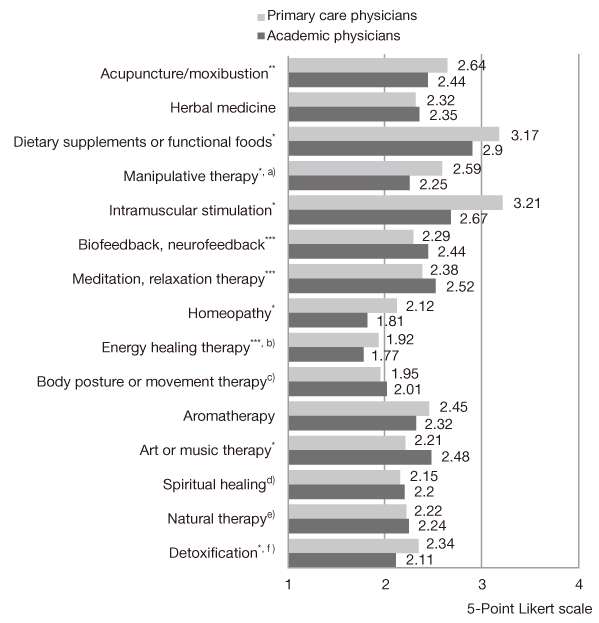
Figure 2
Complementary and alternative medicine modalities with high priority in various situations. PCPs, primary care physicians; APs, academic physicians.

Figure 3
Doctors' discrepant attitude toward complementary and alternative medicine (CAM) use in different situations. Physicians in both groups show significantly more positive attitudes about CAM use of their close acquaintances such as family members, friends or colleagues rather than of their patients. Positive means "recommend CAM use" or "implicit permission"; Negative means "not prohibit, but expressed a concern about side effects", or "strongly prohibited." PCPs, primary care physicians; APs, academic physicians

Table 1
Demographic characteristics
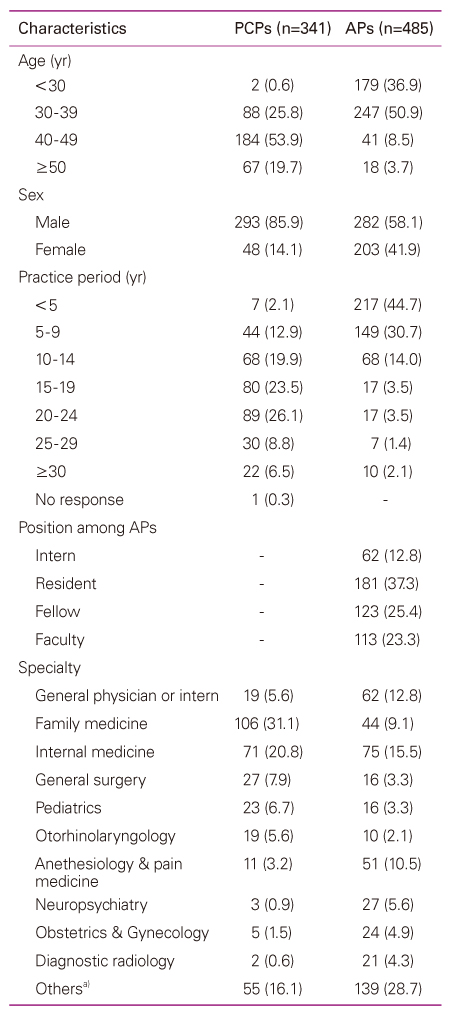
Values are presented as numver (%)
PCPs, primary care physicians; APs, academic physicians.
a)The specialties of orthopedic surgery, urology, ophthalmology, thoracic surgery, rehabilitation medicine, neurosurgery, dermatology, neurology, emergency medicine, laboratory medicine, and clinical pathology.
Table 2
Five-point scale of CAM attitude from 1 (most negative) to 5 (most positive)
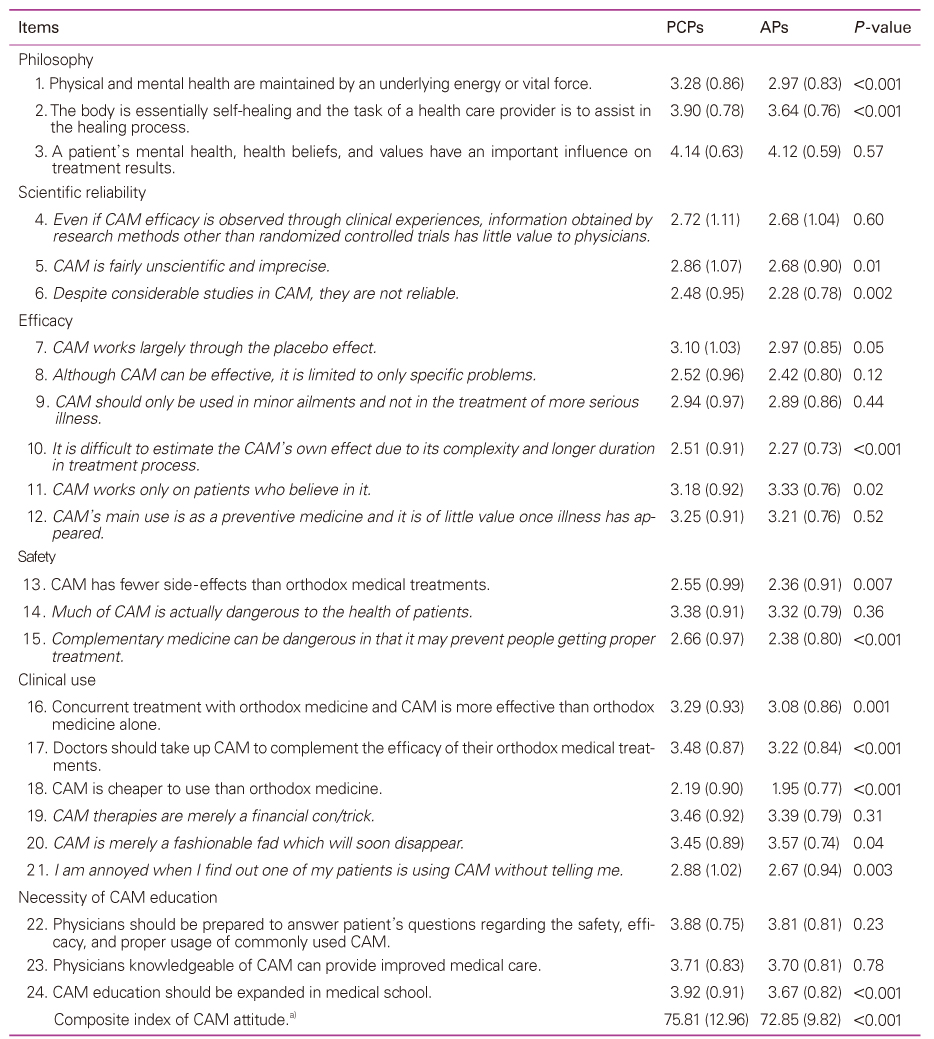
Values are presented as mean (SD). Italicized statements were reversely scored; thus the higher score on the 5-point Likert scale means the more favorable opinion toward CAM in all statements.
CAM, complementary and alternative medicine; PCP, primary care physician; AP, academic physician.
a)Calculated by summing across the 24 rating items.
- TOOLS