|
 |
- Search
| J Korean Med Assoc > Volume 64(3); 2021 > Article |
|
Abstract
Pusan National University Children’s Hospital (PNUCH) opened in November 2008 as the second National Children’s Hospital in Korea and celebrated its 10th anniversary in 2018. In the last decade, birth rates and pediatric populations have been declining sharply and has been more serious in Busan, Ulsan, and Gyeongsangnam-do where the PNUCH is located, affecting the prevalence of index diseases. The number of the index diseases was investigated by year according to changes in the population. Patients who underwent surgery at PNUCH for 10 years were included. Changes in pediatric population and the number of live births were analyzed using the data from Statistics Korea. The number of the index diseases was analyzed retrospectively through the review of electronic medical records. Statistical analysis was performed through Poisson regression. The number of live births and pediatric population decreased from 69,528 to 48,600 (30.1%) and 1,880,284 to 1,444,961 (23.2%), respectively. Operations of pediatric surgery decreased by 32.3% compared to that during the peak season, but the prevalence rate ratio of the pediatric population increased to 1.03 (P<0.001). The number of emergency operation increased due to the largest surge in acute appendicitis operations. Both esophageal atresia and Hirschsprung disease decreased, while hypertrophic pyloric stenosis significantly increased. The absolute number of pediatric surgery cases decreased. However, considering the changes in pediatric population and the number of live births, the relative number of pediatric surgery cases does not changed. The decrease in the number of each disease would be related to the decrease in pediatric population and the number of live births. We should consider the increase of emergency operations such as acute appendicitis.
Pusan National University Children’s Hospital (PNUCH) opened in November 2008 as the second national children’s hospital in Korea and celebrated its 10th anniversary in 2018. The department of pediatric surgery of PNUCH has played a major role as one of the central axes of the hospital.
In the past decade, there have been many changes in the healthcare environment. Owing to advances in medical technology, laparoscopic surgery is also popular in pediatric surgery, and treatments for various diseases have been developed [1,2]. The introduction of a diagnosis-related group and insurance payments for pediatric patients have changed, affecting overall care [3]. However, changes in the birth rate and the pediatric population have been most notable. The birth rate is decreasing rapidly, causing a rapid decrease in the pediatric population. The problem has been more serious in Busan, Ulsan, and Gyeongsangnam-do regions, where the PNUCH is located [4].
This study aimed to investigate the changes in the field of pediatric surgery based on the analysis of index cases. Considering the change in the pediatric population, we compared our results with previous reports according to the prevalence of index cases and reviewed the frequency of emergency surgery.
Patients under the age of 19 who underwent surgery at the department of pediatric surgery of PNUCH from November 2008 to December 2018 were included in this study. Because PNUCH was opened in November 2008 and performed only a few operations in 2008, operations performed in 2008 were included in the total number of cases only; however, population changes were excluded from the investigation. Data on the number of live births and population of Busan, Ulsan, and Gyeongsangnam-do were analyzed using the data from Statistics Korea (http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B8000H&conn_path=I3, http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B040M5&conn_path=I3; accessed April 11, 2019). Index diseases were selected based on those importantly described in the pediatric surgery section of the textbook of the surgery [5]. The authors have added highly prevalent or clinically important diseases after discussion. The number of operations was counted based on the number of surgeries that a patient underwent for a certain disease. If a patient had two or more surgeries because of the same disease, only one operation was counted. A retrospective review of the electronic medical records was performed. The numbers of patients and operations were compared to the pediatric population and the number of live births.
For statistical analysis, Poisson regression analysis was performed using IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA). Poisson regression analysis is a generalized linear model. For groups with the same risk factors, the analysis was based on the supposition that the expected disease incidence remains constant throughout the study period. In general, it can be applied to diseases with an incidence rate of less than 5% of the population. The relative risks of the risk factors on the incidence rate can be identified with a 95% confidence interval. If the confidence interval is ›1, the risk increases significantly, and if it is ‹1, it can be interpreted as a significant decrease. In this study, the prevalence rate ratio (PRR) represents the confidence interval, and when the P-value is ‹0.05, it is considered statistically significant [6].
In 2008, in Busan, Ulsan, and Gyeongsangnam-do regions, the number of live births were close to 70,000, but in 2018, it decreased by approximately 30% to 48,000. The pediatric population under the age of 19 revealed a similar pattern and decreased by 23.1% from 1,880,284 in 2008 to 1,444,961 in 2018.
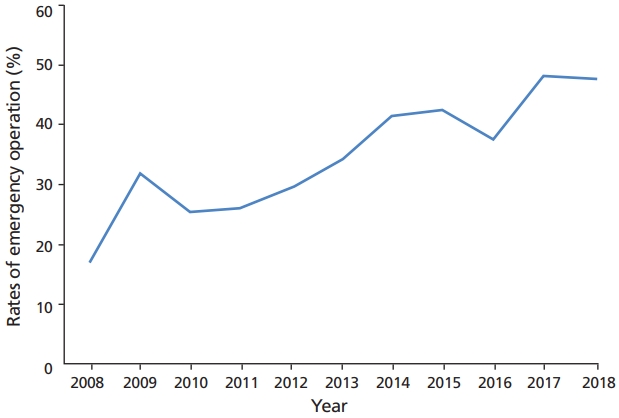
The overall number of surgeries in the department of pediatric surgery of PNUCH peaked at 617 cases in 2014, but then declined by 22.5% in 2018 with a decrease in the pediatric population (Table 1). The PRR was 1.03 (P‹0.001), reflecting the decrease in population, and revealed that the overall number of surgeries was maintained compared to the decrease in population. Even if the overall number of surgeries decreased, the number of emergency operations did not show significant changes, and the proportion of emergency operations was constantly increasing (PRR=1.099, P‹0.001) (Figure 1).
Congenital diaphragmatic hernia (CDH), esophageal atresia (EA) with or without tracheoesophageal fistula, hypertrophic pyloric stenosis (HPS), small bowel atresia (SBA), Hirschsprung disease (HD), anorectal malformation (ARM), necrotizing enterocolitis, meconium-related ileus, choledochal cyst, biliary atresia, solid tumors, and inguinal hernia were selected as index diseases. Acute appendicitis was selected as the representative disease of emergency operations. SBA included duodenal atresia and jejunoileal atresia. HD was only counted for pathologically diagnosed cases. Necrotizing enterocolitis and meconium-related ileus were limited to patients who underwent surgery. Solid tumors included patients who underwent curative or palliative operation for germ cell tumors such as teratoma, neuroblastoma, hepatoblastoma, Ewing’s sarcoma, inflammatory myofibroblastic tumor, ganglioneuroma, and solid pseudopapillary tumor. In most diseases, the annual cases of operation had decreased slightly or not changed, and there were no statistically significant differences in PRR compared to changes in the pediatric population and the number of live births. EA (PRR vs. pediatric population=0.908, P=0.031; PRR vs. live births=0.908, P=-0.035) and HD (PRR vs. pediatric population=0.904, P=0.003; PRR vs. live births=0.904, P=-0.031) were decreased, and a statistically significant increase was observed in HPS (PRR vs. pediatric population=1.072, P=0.018; PRR vs. live births=1.081, P=-0.010). Cases of acute appendicitis, a disease requiring emergency surgery, had increased (PRR=1.076, P‹0.001) compared to the pediatric population (Table 2).
The national surveys of the Korean Association of Pediatric Surgeons in 2001 [7] and 2016 [8] were compared (Table 3). These surveys presented the values of the result with cases/year by surgeon. During the study period, 2.21 surgeons had attended yearly at the department of pediatric surgery at PNUCH. The national survey in 2001 showed fewer EA patients and more HPS patients than those at PNUCH. The number of patients with EA at PNUCH decreased, while the number of patients with HPS had increased gradually during the study period. The distribution of PNUCH patients during the study period may be relatively irregular, and the disease prevalence may have changed. There seemed to have a small number of HD cases overall. The authors also compared data regarding CDH, EA, SBA, malrotations, and ARM, wherein most cases needed treatment during the neonatal period, according to the national survey of neonatal surgery. The number of patients for each disease in the 2016 report seemed to be smaller than the results of 2001 and the current study. It is unclear whether this result was from neonates only, or whether it was because of the actual decline in the pediatric population.
Index diseases in pediatric surgery were defined as diseases that are of great importance in neonatal and pediatric surgery [7,9]. Index diseases generally require special pediatric surgical training for competent performance, in contrast to mundane diseases [10]. Surgical experiences for index diseases are very important not only for training as a pediatric surgical fellow, but also for maintaining competence as a pediatric surgeon [11].
In this study, the PRR of index diseases compared to that in the pediatric population and the number of live births revealed no statistical changes in most diseases, but eventually, the total number of index diseases was reduced. The cases of appendicitis, a common disease, did not decrease, but rather, its PRR compared to that in the pediatric population was increased. In addition, the number and rate of emergency surgeries were maintained or increased, and a decline of pediatric surgical operations could be observed. In North America, the increased rate of common surgeries and the reduction of index diseases are reported among pediatric surgeons, especially young pediatric surgeons, as shown in this study [10,12]. The synergy of the current decrease in the Korean pediatric population and an increase in common operations, such as those in foreign countries, could lead to a decrease in index diseases. In addition, if the frequency of emergency surgeries increases as in this study, there would be a problem in the education of next-generation pediatric surgeons, thereby causing a poor working environment, making it difficult to find applicants for the next generation. It is necessary to recognize that pediatric surgery is essential to establish contingency plans.
The increase in HPS cases and decrease in EA and HD cases were distinctive in this investigation. Determining the cause of these findings is difficult; therefore, further investigations are necessary. It would be considered unsuitable to compare the results of this investigation directly with data from other regions in Korea or other countries, because the distribution of the surrounding medical environment and pediatric surgery hospitals are different, and especially in the case of foreign countries, the differences between race, surrounding environment, lifestyle, and medical environment will be very large. As a reference, we examined the results of a previous survey that focus on index diseases.
Unfortunately, only a very small number of studies have focused on index diseases in pediatric surgery in Korea. Because there are not enough data for statistical investigation, only simple comparisons can be performed. The national surveys by the Korean Association of Pediatric Surgeons in 2001 [7] and 2016 [8] are not completely suitable for comparison. The period of study, range of patients’ age investigated, and methods of surveys were different. However, these studies revealed similarities and differences in disease prevalence between nationwide results [7] and single regional hospitals. These comparisons may explain the convergence to average of the decrease in EA cases, which had a relatively large number in our center, and the increase in HPS cases, which had relatively small numbers. The results of the 2016 study for neonatal surgery [8] were very different from the results of this study, which seemed to be due to the difference between included patients—those under 19 years of age in this study and newborns. However, most patients with CDH, EA, SBA, and ARM are diagnosed in the neonatal period; therefore, it is difficult to explain the large differences between the results of this study and the 2001 study (Table 3).
A study using health insurance claims data from the Korea National Health Insurance Service revealed incidences of some congenital anomalies from 2008 to 2014. The prevalence per 10,000 live births of CDH, EA, SBA, HD, ARM, and biliary atresia were 1.3, 1.5, 3.0, 7.4, 4.5, and 1.7, respectively. ARM showed an increasing trend with 1.05 of PRR, and HD had a decreasing trend, with PRR values of 0.957. Other diseases did not show significant changes [13].
This study had some limitations. Although PNUCH is a central pediatric hospital in this region, it does not treat all patients in the area, and this study would also have been a single-center experience for 10 years. However, it would be meaningful to reveal the total number of patients and the distribution that is affected by changes in the pediatric population and the number of live births changes at the regional National Children’s Hospital. If a national survey will be conducted, these weaknesses can be overcome.
In conclusion, the pediatric population and the number of live births has sharply decreased since 2015 in the Busan, Ulsan, Gyeongsangnam-do regions. The absolute number of operations in the department of pediatric surgery at PNUCH also revealed the same trend of the decrease in the number of live births after 2015. However, relative cases of operations were maintained compared to changes in the pediatric population. EA and HD cases were decreased, and HPS operations were increased significantly, and we should find the reasons. Acute appendicitis and the rate of emergency operations increased and remained high. If these trends would persist nationwide, deterioration in the working conditions of pediatric surgeons could be expected, and countermeasures will be needed.
Acknowledgement
This study was supported by Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital.
Table 1.
Yearly changes of pediatric population of Busan, Ulsan, and Gyeongsangnam-do province and operation of Pusan National University Children's Hospital pediatric surgery
Table 2.
Yearly changes and PRR according to diseases
Table 3.
Comparison of number of cases by number of surgeons and by year with previous studies
| Source | Lee et al. [7] | Kim et al. [8] | Present study |
|---|---|---|---|
| CDH | 1.1 | 0.7 | 1.8 |
| EA | 1.8 | 1.0 | 3.0 |
| HPS | 13.4 | 0.5 | 6.5 |
| SBA | 3.1 | 1.3 | 3.2 |
| Malrotation | 1.5 | 0.6 | 1.9 |
| HD | 9.0 | 0.6 | 5.1 |
| ARM | 10.4 | 2.3 | 8.3 |
| NEC | 1.3 | - | 3.4 |
| Choledochal cyst | 2.2 | 0.2 | 2.5 |
| Biliary atresia | 2.0 | 0.1 | 0.9 |
| Solid tumor | 6.0 | - | 3.0 |
| Inguinal hernia | 30.7a) | - | 87.1 |
| Acute appendicitis | 35.2 | - | 35.3 |
References
1. Kim DY, Kim IS, Kim HY, Nam SH, Park KW, Park WH, Park YJ, Park JH, Park JY, Park JS, Park JY, Boo YJ, Seo JM, Seol JY, Oh JT, Lee NH, Lee MD, Jang JH, Jung KH, Jung SY, Jung SE, Jung SM, Jung EY, Jung JH, Cho MJ, Choi KJ, Choi SJ, Choi SO, Choi SH, Choi YM, Hong J. Minimal invasive surgery: a national survey of its members by the Korean Association of Pediatric Surgeons. J Korean Assoc Pediatr Surg 2014;20:1-6.

2. Kim D. Current status of pediatric minimal invasive surgery (MIS) in Korea. J Minim Invasive Surg 2016;19:84-88.

4. Kang SW. Annual report on the internal migration statistics 2019. Daejeon: Statistics Korea; 2020.
5. Chung DH. Pediatric surgery. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editor. Sabiston textbook of surgery: the biological basis of modern surgical practice. 20th ed. Philadelphia: Elsevier; 2017. p. 1858-1899.
6. Bae JM, Park KH. All illustrated guide to medical statistics using SPSS. Seoul: Hannarae; 2012.
7. Lee MD, Kim SY, Kim WK, Kim IK, Kim SC, Kim SK, Kim JE, Kim JC, Kim HH, Park KW, Park WH, Seo JM, Song YT, Oh SM, Yoo SY, Lee DS, Lee SK, Lee SC, Chung SY, Chung SU, Jung ES, Jung PM, Cho MH, Choi KJ, Choi SO, Choi SH, Han SJ, Huh YS, Hong C, Whang EH. Index cases in pediatric surgery, 2000: national survey by the Korean Association of Pediatric Surgeons. J Korean Assoc Pediatr Surg 2001;7:147-156.


8. Kim DY, Kim SC, Kim SH, Kim HY, Kim HY, Nam SH, Park KW, Park JB, Park JY, Park TJ, Seo JM, Seol JY, Shin JH, Oh JT, Lee MD, Lee SK, Lee SC, Jang EY, Jang HK, Jung SY, Jung SE, Jung SM, Jung YJ, Jung EY, Cho MJ, Choi SJ, Choi SO, Choi SH, Choi YM, Han SJ, Heo TK. Newborns surgery with congenital anomalies: a national survey of its members by Korean Association of Pediatric Surgeons. J Korean Assoc Pediatr Surg 2016;22:1-5.

9. Ravitch MM, Barton BA. The need for pediatric surgeons as determined by the volume of work and the mode of delivery of surgical care. Surgery 1974;76:754-763.

10. Bruns NE, Shah MA, Dorsey AN, Ponsky TA, Soldes OS. Pediatric surgery - a changing field: national trends in pediatric surgical practice. J Pediatr Surg 2016;51:1034-1038.


11. Abdullah F, Salazar JH, Gause CD, Gadepalli S, Biester TW, Azarow KS, Brandt ML, Chung DH, Lund DP, Rescorla FJ, Waldhausen JH, Tracy TF, Fallat ME, Klein MD, Lewis FR, Hirschl RB. Understanding the operative experience of the practicing pediatric surgeon: implications for training and maintaining competency. JAMA Surg 2016;151:735-741.


Peer Reviewers’ Commentary
이 논문은 부산, 울산, 경상남도 지역에서 소아외과 질환의 진료에 있어 거점병원 역할을 수행하고 있는 국립부산어린이병원에서 지난 10년간의 소아외과 수술 경향을 통계분석하여 소아외과 주요 질환인 지표질환의 수술 유병률의 변화를 보여주는 논문이다. 전국의 자료를 분석한 것이 아니므로 전국적인 대표성을 보여주지는 못하지만, 한 지역의 소아외과 의료상황을 상세하게 묘사하고 10년간의 변화 양상을 파악할 수 있다는 측면에서 의미가 있는 논문이다. 우리나라는 급격한 저출산으로 인하여 소아과 및 소아외과 질환에 대한 치료 지표가 변화할 것으로 예상되는 시기이므로, 이 논문은 과거 10년과 비교할 수 있는 지표를 제공하는 측면에서 가치가 있는 논문으로 판단된다.
[정리: 편집위원회]