신종 코로나바이러스감염증-19 초기 대유행이 정형외과 진료에 미친 영향: 한국 단일 의료기관의 경험
The impact of novel COVID-19 initial pandemic on orthopedic healthcare: an experience from a single institution of South Korea
Article information
Trans Abstract
Background
This study was to investigate the cancellation rate and trend of orthopedic surgeries during the novel coronavirus disease 2019 (COVID-19) pandemic. Moreover, we assessed the psychologic status of orthopedic healthcare workers, and investigated the details of the preventive surgeries underwent in COVID-19-positive patients.
Methods
For 3 months after January 20, 2020, cancellation rates of elective surgeries were investigated, and the number of elective surgeries conducted in the same period over the last two years was compared. Four different questionnaires were used to investigate psychologic status among the orthopedic health care workers. We compared the outcomes according to occupation (physician or nurse), and type of work (faculty staff or resident physician). Outcomes according to occupation and type of work were compared. Preventive surgeries underwent in patients who could not wait for the results of the COVID-19 diagnosis were investigated.
Results
Spine and hip surgery had relatively lower cancellation rates, and elective surgeries were significantly reduced. During the initial pandemic, the cancellation rate of orthopedic elective surgeries was significantly higher than in the same period of the previous year and was different for each subdivision depending on the degree of pain or disability. The psychological outcomes were within the normal range and there were no significant differences between groups. After preventive surgery, all medical staff involved in the operation tested negative.
Conclusion
During the COVID-19 pandemic, the cancellation rate of orthopedic elective surgeries was significantly higher than in the same period of the previous year. Orthopedic health care workers did not seem to have significant psychological distress. As a result of the preventive surgery in specialized facilities, all the medical staff who participated in the operation tested negative.
Introduction
Since the initial report of the novel coronavirus disease 2019 (COVID-19) from Wuhan, China in December 2019, the spread of pandemic continues to explode worldwide [1]. Health care workers, including clinicians and nurses from around the world, are struggling to manage the many COVID-19 patients. Since their first confirmed case in January 20 2020, South Korea has been severely burdened with COVID-19, showing a rapid increase in case numbers over the last few months [2,3]. Particularly, the epicenter of Daegu, located in southeastern South Korea, has experienced a rapid spread of COVID-19 that has been attributed to a confirmed case on February 19, 2020, which was related to subsequent super spreading at a church service [2,4,5].
A challenging crisis such as the COVID-19 can cause psychological issues including fright, anxiety, uncertainty, and loneliness that affects not only infected patients, but also the health care workers who treat them [6,7]. During this national disaster, assessing the psychological status of health care workers associated with diagnosis, treatment, and care for COVID-19 patients, as well as considering optimal support for these workers, are issues of top priority [8,9]. Furthermore, the relationship between the type of COVID-19 services provided by a health care worker and degree of psychological stress has not been fully understood. Some studies showed that non-frontline workers have less psychological stress in comparison with frontline workers [10,11], but vice versa in other studies [12,13]. Particularly, in order to minimize the risk and negative influence of this disaster in orthopedic health care, it is necessary to acknowledge the effect of COVID-19 on surgeons’ work and mental status; however, no studies have yet reported an impact of COVID-19 on orthopedic surgeons.
In a pandemic such as COVID-19, orthopedic surgery is not a priority, and thus, appears to be less relevant during this urgent situation. In most countries, elective orthopedic procedures are recommended to be delayed [12,14,15]. Moreover, the demand for orthopedic care has decreased due to regulations such as social distancing and home isolation that prevent the transmission of COVID-19. Nevertheless, some orthopedic emergent surgeries have no choice but to be performed, and in such situations, the preliminary settings or strategies of the operation room (OR) should take extreme measures to reduce the risk of viral transmission [16,17]. However, most countries still have not provided guidance regarding the continuation of orthopedic procedures during the COVID-19 pandemic. Furthermore, to date, there has been a paucity of literature on orthopedic surgery related to COVID-19.
Therefore, the purpose of this study is to investigate the proportion of scheduled elective surgeries that were cancelled over a three-month pandemic period in Daegu, the Korean epicenter of COVID-19, and compare the number of surgeries conducted during this period to the same period in last two years. Moreover, we sought to describe the psychologic parameters in orthopedic healthcare workers. Finally, we tried to investigate whether any preventive surgeries were performed in COVID-positive patients and whether COVID-19 was transmitted to any healthcare workers involved in their care.
Methods
1. Source of data
The present study was approved by the institutional review board of Yeungnam University Medical Center (YUMC 2020-04-054). Data were collected from a single institution at Daegu, the epicenter of COVID-19 in South Korea, for three months since January 20, 2020, when the first case was confirmed in South Korea. All information was retrieved from the institution’s medical records, including detailed information such as primary diagnosis, surgical procedure, use of specialized facilities (including negative pressure environments), whether the operation was performed, and if COVID-19 was diagnosed. During the COVID-19 pandemic, Yeungnam University Medical Center established a guideline to routinely perform a COVID-19 diagnostic test in all patients requiring surgery from the outpatient clinic or emergency room (Table 1). In addition, we assessed the psychological impact of COVID-19 on all orthopedic staff at our institution (16 men and 32 women). We surveyed orthopedic health care workers using four different questionnaires, and informed consent was obtained from all survey participants prior to their enrollment.
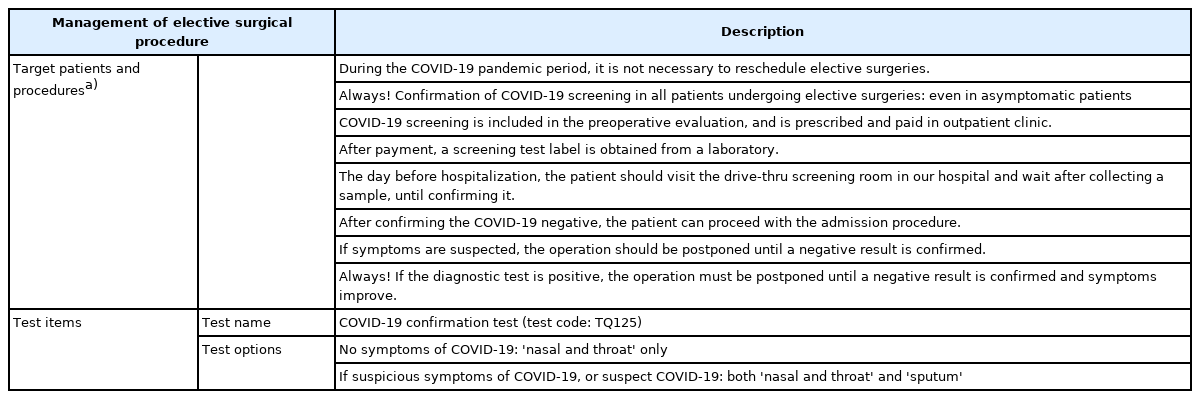
Recommendations from our institution for management of elective surgical procedures during COVID-19 pandemic
Patients requiring urgent procedures that could not wait for COVID-19 results and diagnosis underwent surgical treatment with preventive measures, such as employing a temporary negative pressure room and a mobile negative pressure tent for patient transport in a specific OR complex with special facilities (Figure 1). These patients were relocated to wards based on the results of the COVID-19 diagnosis after surgery.
2. Influence on elective surgeries
“Elective surgery” is defined as a pre-planned procedure that provides medically unnecessary or nonemergent surgery which, if delayed, does not place a patient's immediate health, safety, or wellbeing at risk, or contribute to the worsening of a life-threatening medical condition [12,15]. During events such as a pandemic, cancellation rates of elective surgeries for each orthopedic subdivision were compared. In addition, the difference in the number of surgeries in each subdivision during the same period over the past two years was also compared.
3. Mental health care measures among orthopedic health care workers
In regard to the psychologic impact of the COVID-19 outbreak in South Korea, we assessed the severity of symptoms of anxiety, depression, and distress in orthopedic health care workers of Yeungnam University Medical Center. The survey was conducted for about a month from January 20, 2020, when the number of COVID-19 patients peaked in Daegu, South Korea. Accordingly, we surveyed orthopedic health care workers using four different questionnaires, including the Hamilton aAnxiety rRating sScale (range, 0 to 56) [18], the 22-item impact of event scale-revised (IES-R) scores (range, 0 to 88) [19], the Korean version of the Beck Depression Inventory-II (range, 0 to 63) [20], and the short form-12 health survey including physical and mental components (range, 12 to 58) [21]. The total scores of these measurements were interpreted as follows: Hamilton Anxiety Rating Scale, normal (<18), mild (18 to 24), moderate (25 to 29), severe (≥30) anxiety; IES-R, normal (0 to 8), mild (9 to 25), moderate (26 to 43), and severe (44 to 88) distress; Korean version of the Beck Depression Inventory-II, normal (<9), mild (10 to 15), moderate (16 to 23), severe (≥24) depression. Each category was based on values established in the literature [18-20]. Furthermore, we compared the outcomes according to occupation (physician or nurse), and type of work (faculty staff or resident physician).
4. Outcomes of preventive surgeries
Generally, elective surgeries on non-COVID-19 patients in our institution were assigned to the main OR complex. Patients suspected to have COVID-19 underwent preventive surgery in a specific OR complex separated from the main complex with facilities such as negative pressure environments (maintained at -5.0 to -6.0 Pa) and personal protective equipment (Figure 2) [12,16]. Additionally, patients in need of urgent procedures who could not wait for COVID-19 results and diagnosis underwent preventive surgery in a separate OR complex. During the study period, we investigated the details of preventive surgeries and the presence of postoperative COVID-19 transmission of operation-related staffs.
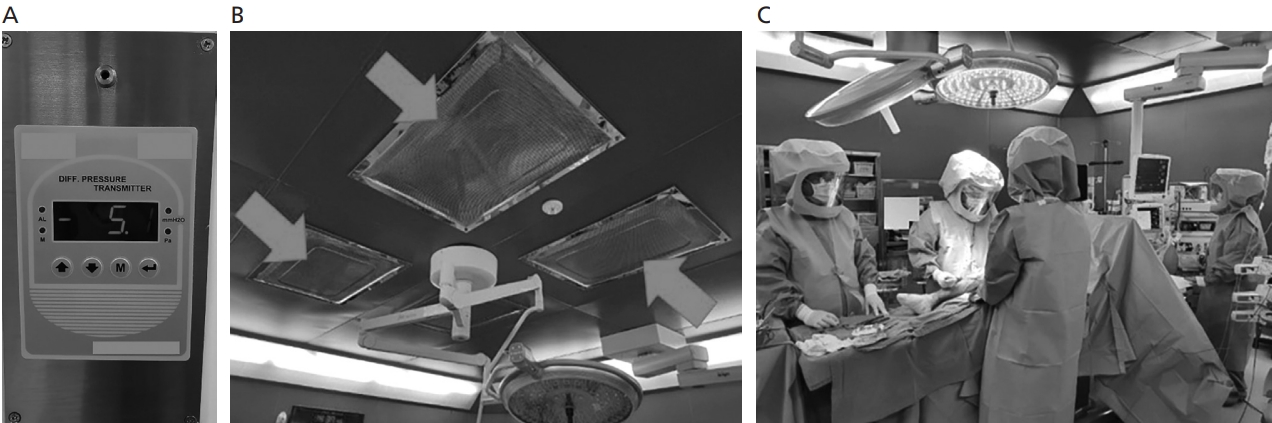
A specific operating room and protective equipments for coronavirus disease 2019. (A,B) Operating room with a negative pressure environment (red arrows) in the isolated specific operating room complex separated from the main complex for elective surgeries. (C) When performing preventive surgery in patients with multiple traumas suspected of having coronavirus disease 2019, all medical staffs involved in the surgery must wear personal protective equipment, such as a protective suit.
5. Statistical analysis
Data analysis was performed using IBM SPSS software (ver. 23.0; IBM Corp., Armonk, NY, USA), and continuous data were expressed as means with ranges. The Kolmogorov-Smirnov test was utilized to evaluate all dependent variables for normality of distribution and equality of variance. Moreover, data was also analyzed using nonparametric tests based on normality. Between the groups, continuous variables were compared by Mann-Whitney U test and Kruskal-Wallis test depending on the normality of distribution. Categorical variables were compared using chi-square or Fisher exact test. A P-value <0.05 was considered statistically significant.
Results
1. Cancellation of elective surgery and changes of surgery conducted
Among a total of 151 elective surgeries during a reference period of January 20, 2020-April 20, 2020, 84 cases (55.6%) were delayed due to COVID-19 and the remaining 67 (44.4%) were conducted as scheduled (Table 2). During the COVID-19 pandemic period compared to the same period in the past two years, elective surgeries at the institution significantly decreased (P=0.003) (Figure 3).
2. Psychological impact on health care workers in orthopedic division
In total, 48 health care workers in the orthopedic division (16 men and 32 women) answered the questionnaire. The average age was 35.9 years (range, 22 to 60 years). All physicians participating in the survey were men, and all nurses were women. Although IES-R showed mild distress, most of psychological outcomes were within the normal range and there were no significant differences between the groups according to occupation or type of work (Table 3).
3. Emergent surgery for patients suspected to have COVID-19
During the study period, a total of 47 preventive surgeries were performed at the hospital. The majority of preventive surgeries (19 cases) were performed in the orthopedic surgery unit, followed by general surgery and other units (Table 4). All patients had a fever of 37.7℃ to 38.7℃, and nine patients had respiratory symptoms such as cough or sputum. Among these, only one patient suffering from a diabetic foot was confirmed as COVID-19-positive after surgery; however, all medical staff involved in the operation tested negative.
Discussion
The most notable findings in the current study indicate that the cancellation rate of elective procedures in the orthopedic department was significantly higher during the COVID-19 pandemic compared to the same period of the previous year or before the outbreak of this virus. Furthermore, the discontinuation of elective procedures was significantly different for each subdivision. During the same period, the mental health status of health care workers in the orthopedic division was mostly within normal limits on psychological questionnaires. Additionally, there were no significant differences in psychological outcomes according to occupation or type of work. Although there was one postoperative patient that tested positive for COVID-19, the virus was not transmitted to health care workers who were involved in the operation, including surgeons.
To date, the cancellation rate of elective surgery in orthopedic divisions during viral epidemic outbreaks such as COVID-19 has not been reported. The cancellation may be due to the public health awareness or individual patient needs. There have been no established guidelines regarding cancellation of orthopedic procedures in South Korea during the COVID-19 pandemic. Since some cases are ambiguous, the guidelines and decision-making often depend on the individual hospital system or surgeon. Meanwhile, several states in the United States have recommended the minimizing, delay, or cancellation of nonessential elective surgical, endoscopic, dental, and orthopedic procedures as much as possible [12,15,22]. In the current study, the cancellation rate in the spine subdivision was the lowest, which is likely due to the high degree of pain and disability of patients, compared to those suffering from knee, foot, or ankle injuries.
Several previous studies have reported on the mental health status of health care workers during viral epidemic outbreaks such as COVID-19, severe acute respiratory syndrome, and Middle East respiratory syndrome [6,7,23,24]. During this period, medical staff in direct contact with infected patients consistently has a fear of infection. Accordingly, such outbreaks of epidemics may cause severe emotional distress, anxiety, depression, and post-traumatic stress among health care workers [6,25]. Particularly, it has been reported that clinicians may have more fundamental psychological distress from such epidemics compared to other health care professionals [11,26]. However, in the current study, health care workers in the orthopedic division did not demonstrate severe mental health issues according to the conducted surveys. Moreover, although some studies reported psychological differences according to type or level of work [10,11], there were no significant differences in the current study. It is thought that health care workers in orthopedic surgery, who are non-frontline workers that rarely directly treat COVID-19 patients, may not have severe emotional distress. Additionally, the reduction in demand for orthopedic care due to the COVID-19 pandemic seems to benefit orthopedic health care workers in regard to mental health. A recent study reported some advantages for orthopedic surgeons during this calamity, including more time for personal stress relief, time away from the radiation exposure, the opportunity to finish pending research, and more time with their family [27].
When performing surgery on patients suspected of having COVID-19, specialized facilities such as isolation OR, negative pressure mechanisms, and personal protective equipment are essential [16]. These measures can optimize the quality of care provided to patients infected with COVID-19 and minimize the risk of viral transmission to other patients or health care workers. We performed preventive surgery in patients who were suspected of having COVID-19 without confirming the results of the diagnosis due to a time-sensitive urgency for surgery. Although one patient was confirmed positive after surgery, the virus was not transmitted to the medical staff involved.
This study has some limitations. First, the scope of the study is limited. This study collected data related to orthopedic surgery at the main medical institution in Daegu. Therefore, it may be difficult to generalize the results of the current study to all regions of South Korea or Asia. Nevertheless, data from Daegu, the epicenter of South Korea, a representative country of the early COVID-19 outbreak, can be a good reference for medical staff in other regions. Second, since the study was based on three months of data since the first confirmation of COVID-19, it lacks long-term follow-up results. Although the current mental health status of orthopedic surgeons is reported to have no major problems, it is possible that health care workers may experience a severe deterioration in psychological state as the pandemic continues. Therefore, follow-up of long-term psychological symptoms for these subjects is needed.
Nevertheless, this study suggests some valuable information for many health care workers, including orthopedists, during the COVID-19 pandemic. (1) To date, this study is the first to report the cancellation rate of elective procedures in orthopedic division during the COVID-19 pandemic; (2) Health care workers, such as orthopedic surgeons, who rarely treat patients infected with COVID-19 directly, report to have less psychologic stress. Furthermore, it showed that the pandemic may be a positive factor in mental health for orthopedic health care workers, as their overall workload was reduced; and (3) In patients suspected of having COVID-19, performing preventive surgery in special facilities equipped with negative pressure environments or personal protective equipment could prevent the transmission to involved health care workers.
In conclusion, during the COVID-19 pandemic, the cancellation rate of orthopedic elective surgeries was significantly higher than in the same period of the previous year and differed for each subdivision depending on the degree of pain or disability reported by patients. Health care workers in the orthopedic division did not report significant psychological distress As a result of the preventive surgery in specialized facilities, all the medical staff who participated in the operation tested negative.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2021R1A6A1A03040177).