Easy sedation anesthesia guide for non-anesthetic medical personnel
Article information
Abstract
Abstract
Currently, sedation anesthesia is increasingly used in many medical fields, from gastroscopy to medical imaging. The demand for sedation anesthesia is expected to increase gradually with increasing number of day surgeries and increased expectations from medical services. The demand for sedation anesthesia is considerably higher than the available pool of anesthesiologists; therefore, in a significant number of cases, sedation anesthesia is induced by non-anesthesiologists. However, there is no systematic provision of education or expertise for non-anesthesiologists in delivering sedation anesthesia. In cases of non-anesthesiologists inducing anesthesia, social controversy is often caused by medical accidents and substance abuse. In this review, I have briefly summarized what non-anesthesiologists should know about sedation anesthesia and have presented guidelines simplifying sedation anesthesia for non-anesthesia medical personnel.
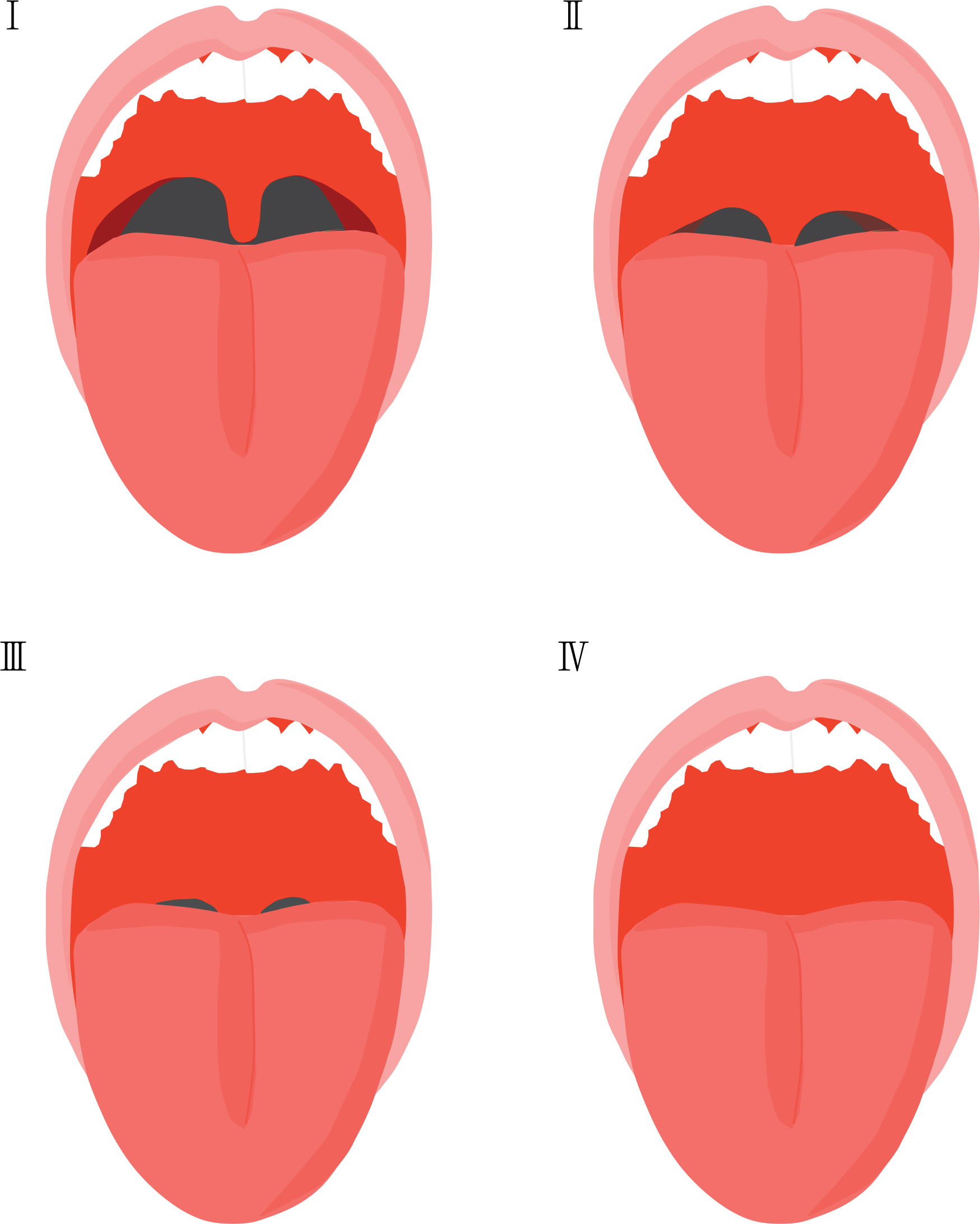
Modified Mallampati classification. Class I: soft palate, fauces, uvula, pillars are visible. Class II: soft palate, fauces, the part of uvula are visible. Class III: soft palate, the bottom of uvula are visible. Class IV: only hard palate is visible. Bair AE, Caravelli R, Tyler K, Laurin EG. Feasibility of the preoperative Mallampati airway assessment in emergency department patients. J Emerg Med 2010;38:677-680. Illustration by Min TJ.
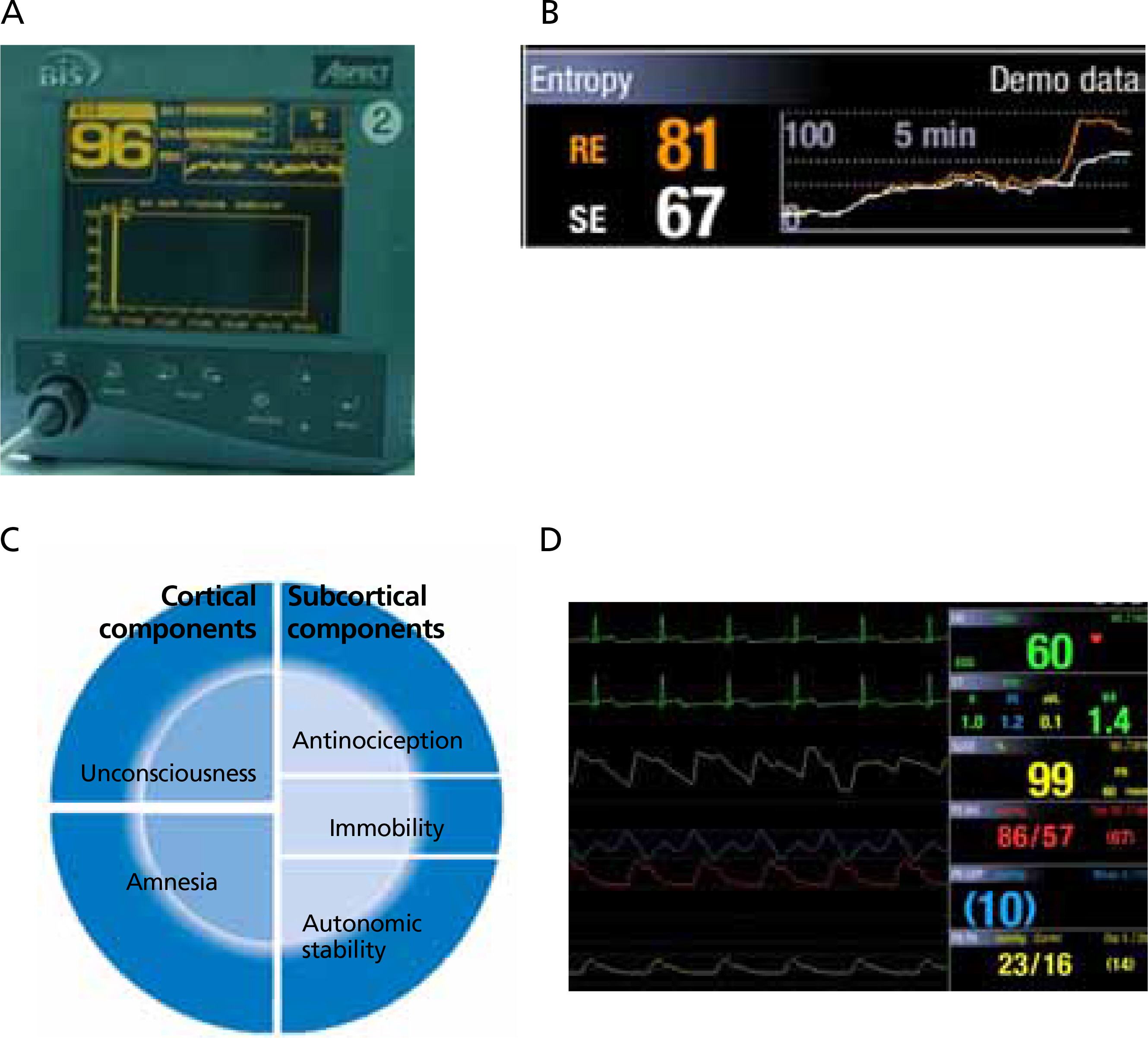
Anesthetic depth measuring systems. (A) Bispectral index, (B) entropy, (C) schematic diagram for sedation depth, and (D) autonomic indicators.

End-tidal CO2 monitoring device. (A) Mask end-tidal CO2 monitoring device. (B) Nasal prong end-tidal CO2 monitoring device. Illustration by Min TJ.
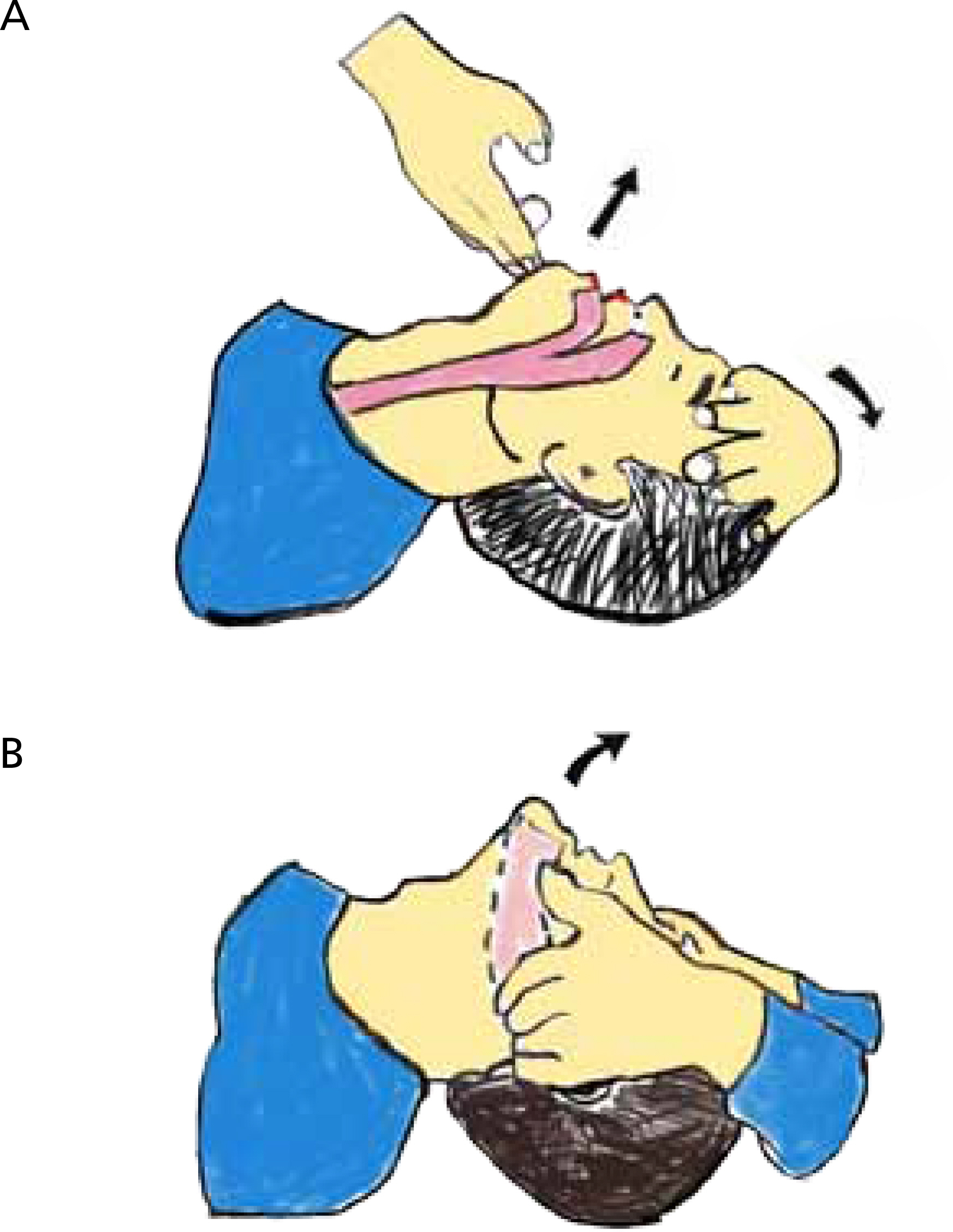
Airway secure maneuvers. (A) Head tilt chin-lift maneuver. (B) Jaw-thrust maneuver. Pratice Paramedicine, July 5, 2018. Illustration by Min TJ.


